Transparent Peer Review
Download the complete Review Process [PDF] including:
- reviews
- authors' reply
- editorial decisions
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Wallis, C. (n.d.). Why Some People Get Terribly Sick from COVID-19. Scientific American. Retrieved August 24, 2020, from https://www.scientificamerican.com/article/why-some-people-get-terribly-sick-from-covid-19/
As well as the discussion about what is really meant by a ‘domain of one’s own‘
Societies have been inexorably been moving toward interdependence. More and more people specialize and sub-specialize into smaller fragments of the work that we do. As a result, we become more interdependent on the work of others to underpin our own. This makes the worry about renting a domain seem somewhat disingenuous, particularly when we can reasonably rely on the underlying structures to work to keep our domains in place.
Perhaps re-framing this idea may be worthwhile. While it may seem that we own our bodies (at least in modern liberal democracies, for the moment), a large portion of our bodies are comprised of bacteria which are simultaneously both separate and a part of us and who we are. The symbiosis between people and their bacteria has been going on so long and generally so consistently we don't realize that the interdependence even exists anymore. No one walks around talking about how they're renting their bacteria.
Eventually we'll get to a point where our interdependence on domain registrars and hosts becomes the same sort of symbiotic interdependence.
Another useful analogy is to look at our interdependence on all the other pieces in our lives which we don't own or directly control, but which still allow us to live and exist.
People only tend to notice the major breakdowns of these bits of our interdependence. Recently there has been a lot of political turmoil and strife in the United States because politicians have become more self-centered and focused on their own needs, wants, and desire for power that they aren't serving the majority of people. When our representatives don't do their best work at representing their constituencies, major breakdowns in our interdependence occur. We need to be able to rely on scientists to do their best work to inform politicians who we need to be able to trust to do their best work to improve our lives and the general welfare. When the breakdown happens it creates issues to the individual bodies that make up the society as well as the body of the society itself.
Who's renting who in this scenario?
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Center for Infectious Disease Dynamics—YouTube. (n.d.). Retrieved 21 February 2021, from https://www.youtube.com/channel/UC1dZp4v6sF2jKjutJguk7ng/videos?view=0&sort=da&flow=grid&view_as=subscriber
Fredericks DN, & Relman DA (1996). Sequence-based identification of microbial pathogens: a reconsideration of Koch’s postulates. Clinical microbiology reviews, 9 (1), 18-33 PMID: 8665474
Repostulation of Koch's rules in the era of the virueses.
Proteins are made up of building blocks called amino acids. N501Y means that the 501st amino acid was originally an N, which stands for the amino acid asparagine, but has been changed to a Y, which stands for tyrosine.
The takeaway: Amino acids, represented by single letters such as N or Y make up proteins which are part of the coronavirus (as well as other biology such as animals, plants, microorganisms, etc.). Mutations are written with the original amino acid letter followed by the number of the amino acid and the new amino acid letter.
The claim: Proteins are made up of building blocks called amino acids. N501Y means that the 501st amino acid was originally an N, which stands for the amino acid asparagine, but has been changed to a Y, which stands for tyrosine.
The evidence:
Coronavirus is made up of greater than 20 proteins (1). The spike protein helps coronavirus attach and enter human cells which leads to infection and disease (1). The spike protein on SARS-CoV-2, the virus that causes COVID-19, is the target of many antibodies produced by the human body to fight the SARS-CoV-2 infection (2). Changes in the spike protein sequence may necessitate a change in the human immune system to produce antibodies which stop SARS-CoV-2 from infecting human cells. Changes in the amino acid sequence are written as was stated in the claim: original amino acid, number of the amino acid in the sequence, new amino acid.
Sources:
Johnson: Earlier I interviewed you about patrilocal residence patterns and how that alters women’s sexual choices. In contrast, matrilocal societies are more likely to be egalitarian. What are the factors that lead to the differences between these two systems?Hrdy: I think in societies where women have more say, and that does tend to be in societies that are matrilocal and with matrilineal descent or where, as it is among many small scale hunter-gatherers, you have porous social boundaries and flexible residence patterns. If I had to say what kind of residence patterns our ancestors had it would have been very flexible, what Frank Marlowe calls multilocal.
Matrilocality, matrilinearity and egailitarianism.
“Half of what you learned in college is wrong,” my biology professor, David Lange, once said. “Problem is, we don’t know which half.”
Very interesting that a biology professor believes that 50% of what we learn can be wrong.
Schleiss says a better analogy for COVID-19 is the mumps. For more than 45 years, we’ve had a very effective vaccine for measles, mumps, and rubella (which are also RNA viruses).
The takeaway: Even though mutations happen in all virus, vaccines still work. Current evidence about SARS-CoV-2 indicates that an effective COVID-19 vaccine can be obtained, and that it should be able to provide immunity against the virus.
The claim: A better analogy for COVID-19 is the mumps. For more than 45 years, we’ve had a very effective vaccine for measles, mumps, and rubella (which are also RNA viruses).
The evidence: We are all imperfect and we all make mistakes. For a virus, a mistake means the introduction of a mutation in its sequence, and RNA viruses (like the flu, mumps, measles virus, and SARS-CoV-2) have the highest error rates in nature. Mutations are indispensable for viral survival and evolution; this property is believed to benefit the viral population, allowing it to adapt and respond to different complex environments encountered during spread between hosts, within organs and tissues, and in response to the pressure of the host immune response [1]. How fast a virus is changing can be estimated by measuring its mutation rate, and then they can be classified as changing fast – high mutation rate – like HIV or Influenza, or as stable, like measles or mumps virus. SARS-CoV-2 has a mutation rate three times slower than the flu virus [2], but it's still changing faster than the mumps virus (the mutation rate of influenza is more than 10 times higher than mumps) [3]. Of course, how fast a virus can change has implications in the efficacy of treatments and vaccines, but it's not the only determinant. Even though mutations happen in all viruses, vaccines still work. A great example is the measles virus, as the antigenic composition of the vaccine (the molecules that “wake up” the immune system) used to prevent it has remained efficient since it was developed, in the 1960s, and confers protection against the 24 circulating genotypes [4]. The same is true for the mumps virus, with a vaccine that has been efficient for many decades [5]. Sequencing data suggest that coronaviruses change more slowly than most other RNA viruses, probably because of a viral ‘proofreading’ activity that corrects all the copying mistakes [6]. Taken together, all this evidence indicates that an effective COVID-19 vaccine can be obtained, and that it should be able to provide lasting immunity against the virus.
Sources:<br> 1
2 SARS-CoV-2 mutation rate: 1.26 x 10-3 substitutions/site/year
3 Influenza (flu-virus) mutation rate: 3.68 x 10-3 substitutions/site/year. Mumps mutation rate: 2.98 × 10−4 substitutions/site/year
Kits rock! But understanding what is going on at each stage of the protocol provided with the kit really helps with troubleshooting and modification.
Ideas on how to analyze and predict network behavior have been informed by concepts arising from the computational and social sciences, which are themselves increasingly concerned with understanding networks. The interesting thing about these ideas is that they work at scales ranging from the molecular to the population level.
scale free networks perhaps?
I had bookmarked this article in the form of tearing out and keeping a paper copy of it in my to read pile back in 2008. Finally getting around to reading it today. It's still an interesting introduction to the broader area which has moved forward, but not significantly enough to date the entire area.
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Researchers offer first proof that Ultraviolet C light with a 222 nm wavelength — which is safer to use around humans — effectively kills the SARS-CoV-2 virus.
Take Away: Most germicidal ultraviolet (UV) lamps emit a wavelength of around 254 nm. While these are very effective means of sterilization, they are also damaging to human skin and eyes and therefore are used in unoccupied spaces. However, a recent study has shown that a safer form of UV light at a wavelength of 222 nm is effective in killing SARS-CoV-2 virus in vitro.
The Claim: Researchers offer first proof that Ultraviolet C light with a 222 nm wavelength — which is safer to use around humans — effectively kills the SARS-CoV-2 virus.
The Evidence: The authors reference the safety of 222 nm UV light, and there are many studies to support this claim. 222 nm UV light has been shown to not cause DNA damage or skin lesions even at higher doses and for longer exposure times than used here (1, 2).
In the study referenced, researchers at Hiroshima University exposed SARS-CoV-2 virus to low dosage 222 nm UV light and subsequently measured the amount of viable virus (3). They found that exposure of 0.1 mW/cm^2 for 30 seconds reduced the amount of viable virus by 99.7%. However, as the authors note, this study was performed using virus plated on a dish in a hood, and translation of these results to a public setting is unclear. For instance, in a hospital, there are many different types of surfaces and direct/consistent exposure to the UV light might not be feasible. While this study is promising, additional studies need to be done before promoting this as a safe and effective means of killing SARS-CoV-2 in an occupied environment.
Sources: 1) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6059456/
2) https://onlinelibrary.wiley.com/doi/abs/10.1111/php.13269
The lowest value for false positive rate was 0.8%. Allow me to explain the impact of a false positive rate of 0.8% on Pillar 2. We return to our 10,000 people who’ve volunteered to get tested, and the expected ten with virus (0.1% prevalence or 1:1000) have been identified by the PCR test. But now we’ve to calculate how many false positives are to accompanying them. The shocking answer is 80. 80 is 0.8% of 10,000. That’s how many false positives you’d get every time you were to use a Pillar 2 test on a group of that size.
Take Away: The exact frequency of false positive test results for COVID-19 is unknown. Real world data on COVID-19 testing suggests that rigorous testing regimes likely produce fewer than 1 in 10,000 (<0.01%) false positives, orders of magnitude below the frequency proposed here.
The Claim: The reported numbers for new COVID-19 cases are overblown due to a false positive rate of 0.8%
The Evidence: In this opinion article, the author correctly conveys the concern that for large testing strategies, case rates could become inflated if there is (a) a high false positive rate for the test and (b) there is a very low prevalence of the virus within the population. The false positive rate proposed by the author is 0.8%, based on the "lowest value" for similar tests given by a briefing to the UK's Scientific Advisory Group for Emergencies (1).
In fact, the briefing states that, based on another analysis, among false positive rates for 43 external quality assessments, the interquartile range for false positive rate was 0.8-4.0%. The actual lowest value for false positive rate from this study was 0% (2).
An upper limit for false positive rate can also be estimated from the number of tests conducted per confirmed COVID-19 case. In countries with low infection rates that have conducted widespread testing, such as Vietnam and New Zealand, at multiple periods throughout the pandemic they have achieved over 10,000 tests per positive case (3). Even if every single positive was false, the false positive rate would be below 0.01%.
The prevalence of the virus within a population being tested can affect the positive predictive value of a test, which is the likelihood that a positive result is due to a true infection. The author here assumes the current prevalence of COVID-19 in the UK is 1 in 1,000 and the expected rate of positive results is 0.1%. Data from the University of Oxford and the Global Change Data Lab show that the current (Sept. 22, 2020) share of daily COVID-19 tests that are positive in the UK is around 1.7% (4). Therefore, based on real world data, the probability that a patient is positive for the test and does have the disease is 99.4%.
(2) https://www.medrxiv.org/content/10.1101/2020.04.26.20080911v3.full.pdf+html
He added that while it would not be possible to check every test to see whether there was active virus, the likelihood of false positive results could be reduced if scientists could work out where the cut-off point should be.
Take Away: This is an incorrect usage of the term "false positive." A positive PCR test result from a recovered infection is a valid and true positive.
Claim: PCR tests for SARS-CoV-2 give false positive results when there is no active virus.
Evidence: The diagnostic PCR tests currently in widespread use are designed to detect the presence of the SARS-CoV-2 viral RNA in a clinical sample. The RNA is only a part of the complete virus and is not infectious on its own. Research has shown that viral RNA can be detected in some samples up to 12 weeks after onset of symptoms (1). In other words, this is like testing if an oven is warmer than the room temperature - it could be hot even after it has been turned off.
By definition, in the context of SARS-CoV-2 PCR tests, a "false positive" means that a test result is deemed positive when in reality there was no viral RNA in the sample. If a person is recovering from an infection, gets tested, and then is given a positive test result, that is a true positive regardless of whether they are infectious or not.
Sources: 1) https://www.cdc.gov/coronavirus/2019-ncov/hcp/duration-isolation.html
Take away: People are infectious for only part of the time they test positive. The tests for COVID-19 were granted emergency status by the FDA so some debate concerning the most ideal number of cycles is to be expected. It is worth noting that the FDA has the disclaimer "Negative results do not preclude 2019-nCoV infection and should not be used as the sole basis for treatment or other patient management decisions. Negative results must be combined with clinical observations, patient history, and epidemiological information (2)."
The claim: Up to 90 percent of people diagnosed with coronavirus may not be carrying enough of it to infect anyone else
The evidence: Per Walsh et al. (1), SARS-CoV-2 virus (COVID-19) is most likely infectious if the number of PCR cycles is <24 and the symptom onset to test is <8 days. RT-PCR detects the RNA, not the infectious virus. Therefore, setting the cycle threshold at 37-40 cycles will most likely result in detecting some samples with virus which is not infectious. As the PCR tests were granted emergency use by the FDA (samples include 2-9), it is not surprising that some debate exists currently about where the cycle threshold should be. Thresholds need to be set and validated for dozens of PCR tests currently in use. If identifying only infectious individuals is the goal, a lower cycle number may be justified. If detection of as many cases as possible to get closer to the most accurate death rate is the goal, setting the cycle threshold at 37-40 makes sense. A lower threshold will result in fewer COVID-19 positive samples being identified. It is worth noting that the emergency use approval granted by the FDA includes the disclaimer that a negative test does not guarantee that a person is not infected with COVID-19. RNA degrades easily. If samples are not kept cold or properly processed, the virus can degrade and result in a false negative result.
Source: 1 https://academic.oup.com/cid/advance-article/doi/10.1093/cid/ciaa638/5842165
2 https://www.fda.gov/media/134922/download
3 https://www.fda.gov/media/138150/download
4 https://www.fda.gov/media/137120/download
5 https://www.fda.gov/media/136231/download
6 https://www.fda.gov/media/136472/download
7 https://www.fda.gov/media/139279/download
Your Coronavirus Test Is Positive. Maybe It Shouldn’t Be.
Take Away: Diagnostic tests are most useful when they are both sensitive and rapid. The sensitivity of SARS-CoV-2 PCR tests is not the issue, but rather the time it takes to get a result. Additionally, the "90%" statistic is likely misleading due to the data source and not generalisable to all testing results.
The Claim: The usual PCR diagnostic tests may be too sensitive and too slow, with up to 90% of positive cases due to trace amounts of virus.
The Evidence: Polymerase Chain Reaction (PCR)-based tests, which are currently in the most widespread use for detection of SARS-CoV-2 RNA, involves a molecular process that amplifies target DNA sequences in repeated temperature-dependent cycles. The amount of target DNA is measured after each cycle and the number of the cycle when the target can be reliably detected is often referred to as the cycle threshold (Ct). The Ct value is proportional to the amount of starting DNA in the sample and can be used to estimate the viral load of a patient. In some ways this is like a teacher making photocopies of a chapter from a textbook until they have enough for all their students.
However, Ct values are relative measurements and need to be directly compared to controls for every sample - a Ct value taken alone can be meaningless. For instance, consider an infected patient who is tested twice: the first time they are gently swabbed and the sample is relatively dilute, the second time they are vigorously swabbed and the sample is relatively concentrated. The resulting Ct values could be drastically different. Therefore, Ct values need to be considered carefully in the proper context for making medical or policy decisions. The FDA also recommends that a PCR result alone should not be used to determine infection status.
Positive results are indicative of the presence of SARS-CoV-2 RNA; clinical correlation with patient history and other diagnostic information is necessary to determine patient infection status. (1)
Current PCR test results are generally given as a binary positive/negative based on a cutoff value for Ct. The cutoff needs to be determined based on the performance of each individually developed SARS-CoV-2 test, of which there are currently over 160 that have been granted emergency use authorization by the FDA (2). Based on unpublished data from the CDC, setting a stringent Ct cutoff of 30 could return negative results in patients who are both infected and potentially infectious (3 Fig 5). Furthermore, a 30 cycle cutoff would return invalid results for samples which are too diluted. Based on the same CDC data, up to 30% of potentially infectious patients would get invalid results and need to be re-swabbed, thereby extending the time between getting infected and getting a positive result.
The period of time when RNA from SARS-CoV-2 can be detected (and a positive PCR test result returned) may extend up to 12 weeks after recovery, with Ct values trending higher over time (3,4). According to The New York Times article, they looked at Ct values from people who tested positive in Massachusetts in July and found 85-90% of results had Ct values greater than 30. The epidemiology of COVID-19 is highly time and region dependent. Massachusetts had a peak in COVID-19 hospitalizations on April 21 (5), which is 9-12 weeks prior to the testing data analyzed by The NY Times. Therefore, the detection of a large proportion of people with lingering viral RNA is not surprising. These results are likely not universal and can not be applied to other regions, especially where community spread is still significant.
Sources:
(1) https://www.fda.gov/media/135900/download
(3) https://www.cdc.gov/coronavirus/2019-ncov/hcp/duration-isolation.html
(4) Li N, Wang X, Lv T. Prolonged SARS-CoV-2 RNA Shedding: Not a Rare Phenomenon. J Med Virol 2020 Apr 29. doi: 10.1002/jmv.25952.
(5) https://www.bostonherald.com/2020/05/22/massachusetts-finally-seeing-downward-coronavirus-trends/
If we are now going to hold our nation hostage because of this obsession over PCR (polymerase chain reaction) swab tests, we should at the very least make certain they’re accurate. What happens when we have expedited and chaotic test results driving an epidemic curve rather than actual symptoms? You get what happened to Ohio Governor Mike DeWine last Thursday. He tested positive for the virus after experiencing absolutely no symptoms. But because he is such a VIP, he got a second, more accurate test that showed he was in fact negative for SARS-CoV-2. The same thing happened to Detroit Lions quarterback Matthew Stafford, who tested negative after receiving a false positive and was therefore allowed out of coronavirus prison.
Take away: Current polymerase chain reaction (PCR) testing technology is very sensitive and specific. Even for rapidly developed new tests for the novel coronavirus, SARS-CoV-2, available clinical data indicates they are highly accurate.
The claim: SARS-CoV-2 testing is unreliable and plagued by false positive results.
The evidence: Any diagnostic test has some degree of error that is typically very low for FDA approved products. For SARS-CoV-2 tests, which detect the presence of the virus that causes COVID-19, although rare, it is possible to get a positive result when you may not have been exposed or infected by the virus. In other words, a false positive. So how frequently do false positives occur?
There is no universal false positive rate for SARS-CoV-2 test results because there are dozens of different tests that have been developed and deployed, each with their own error rate. As of August 26, 2020, there are 146 commercial diagnostic tests that have received emergency use authorization from the FDA. Data from clinical performance testing submitted to the FDA indicates that PCR tests are highly accurate. For example, the specific PCR test mentioned by the author, Quest Diagnostics SARS-CoV-2 rRT-PCR, obtained 100% correct results in clinical evaluation studies (n = 60), and 100% true negative results in a random population of samples from before the pandemic (n = 72).
Additional considerations: In addition to PCR technology-based tests, which detect the viral RNA genome and require lab processing, there are antigen tests, which use antibodies to detect viral proteins and can be rapidly performed in point-of-care settings. Antigen tests are much easier to perform than PCR tests, but they can be less sensitive. For example, the LumiraDx SARS-CoV-2 Ag Test, when compared to PCR, has an overall agreement of 96.9%.
The author provides two anecdotes of high-profile personnel who obtained false positive test results. For the Ohio Governor, his initial positive was from an antigen test, not a PCR test. The NFL quarterback is part of a unique population that is presumed to be largely SARS-CoV-2 negative but is being tested frequently and repeatedly. This scenario increases the probability that a positive test result may be false. However, the NFL in early August said it has conducted over 75,000 tests, so unless there are many additional cases of false positives, this suggests that their testing methodology is over 99.99% accurate.
HARs are short stretches of DNA that while conserved in other species, underwent rapid evolution in humans following our split with chimpanzees, presumably since they provided some benefit specific to our species. Rather than encoding for proteins themselves, HARs often help regulate neighboring genes. Since both schizophrenia and HARs appear to be for the most part human-specific, the researchers wondered if there might be a connection between the two.dfp.loadAds("right2","MPU2","dfp-right2-article-1")Advertisement
Schizophrenia is unique to humans. There are also regions that human and other species have, but have undergone more rapid evolution in humans called Human Accelerated regions (HAR).
Maybe these HARs and Schizophrenia are linked.
Also HARs are regions whose purpose is to regulate the expression of other genes, not so much directly code for a protein.
COVID-19 first appeared in a group of Chinese miners in 2012
Take away: The COVID-19 virus (SARS-CoV2) did not exist in 2012, however a related virus was isolated from bats in 2013.
The claim: The same virus that is causing the COVID-19 pandemic existed in miners in 2012.
The evidence:RaTG13, a virus that was isolated from bats by the Wuhan Institute of Virology in 2013 is the closest known relative to SARS-CoV2, the virus that causes COVID-19 (Ge 2016, Zhou 2020). This bat virus is not the same virus as SARS-CoV2, but is closely related (96% identical DNA). The virus was isolated from bats, not humans. However, it was isolated from a cave near where workers the previous year became sick and some died, and may be linked to the illnesses. The SARS-CoV2 virus shows a number of key adaptations that likely makes it much more infectious in humans than the related bat virus (Wrobel, 2020).
Source:
Ge XY, Wang N, Zhang W, Hu B, Li B, Zhang YZ, Zhou JH, Luo CM, Yang XL, Wu LJ, Wang B. Coexistence of multiple coronaviruses in several bat colonies in an abandoned mineshaft. Virologica Sinica. 2016 Feb 1;31(1):31-40.
Zhou P, Yang XL, Wang XG, Hu B, Zhang L, Zhang W, Si HR, Zhu Y, Li B, Huang CL, Chen HD. A pneumonia outbreak associated with a new coronavirus of probable bat origin. nature. 2020 Mar;579(7798):270-3.
Wrobel AG, Benton DJ, Xu P, Roustan C, Martin SR, Rosenthal PB, Skehel JJ, Gamblin SJ. SARS-CoV-2 and bat RaTG13 spike glycoprotein structures inform on virus evolution and furin-cleavage effects. Nature Structural & Molecular Biology. 2020 Aug;27(8):763-7.
Crespi, S., Wadman, M., (2020). Why men may have more severe COVID-19 symptoms, and using bacteria to track contaminated food. Science | AAAS. https://www.sciencemag.org/podcast/why-men-may-have-more-severe-covid-19-symptoms-and-using-bacteria-track-contaminated-food?utm_campaign=SciMag&utm_source=JHubbard&utm_medium=Twitter
The vaccine uses messenger RNA (mRNA), which are cells used to build proteins -- in this case, the proteins that are needed to build the coronavirus' spike protein, which the virus uses to attach itself to and infect human cells. Once the immune system learns to recognize this target -- thanks to the vaccine -- it can mount a response faster than if it encountered the virus for the first time due to an infection.
This explanation is garbled and misstated. Genetic material is stored in DNA in the nucleus of the cell. Messenger RNA (mRNA) molecules carry the information stored within the DNA to the rest of the cell. Both DNA and RNA are a type of molecule called a "nucleic acid." Once outside the nucleus, the information in the messenger RNA can then be read, or "translated," to create proteins, such as the spike protein used by SARS-CoV-2. These proteins in turn carry out a wide variety of tasks that allow cells to function. This process is known as the "Central Dogma of Molecular Biology".
Bristol, U. of. (n.d.). Avon Longitudinal Study of Parents and Children | Avon Longitudinal Study of Parents and Children | University of Bristol. University of Bristol. Retrieved July 18, 2020, from http://www.bristol.ac.uk/alspac/
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Download the complete Review Process [PDF] including:
Rahmani P, Peruani F, Romanczuk P (2020) Flocking in complex environments—Attention trade-offs in collective information processing. PLoS Comput Biol 16(4): e1007697. https://doi.org/10.1371/journal.pcbi.1007697
Definition: Unit that can be assigned to a group of living beings according to certain criteria. Most of the time, this expresses itself through a separate name for this group.
In 1970 Michener et al. defined "systematic biology" and "taxonomy" (terms that are often confused and used interchangeably) in relationship to one another as follows:
Prasad, S., Knight, E. L., Sarkar, A., Welker, K. M., Lassetter, B., & Mehta, P. (2020, May 6). Testosterone fluctuations in response to a democratic election predict partisan attitudes toward the elected leader. https://doi.org/10.31234/osf.io/w6rz9
Vasiliauskaite, V., & Rosas, F. E. (2020). Understanding complexity via network theory: A gentle introduction. ArXiv:2004.14845 [Physics]. http://arxiv.org/abs/2004.14845
Small-scale biological theories, such as those describing membrane and protein interactions, can be predictive because the relevant processes are dominated by physical constraints, such as diffusion, hydrophobicity and entropy. The problem is that these types of theories do not scale, and become far less predictive as we increase the complexity of the system.
Evidence Tracker: COVID-19
The molecular analysis also show that the SARS-Cov2 virus is active and replicates already in the nasopharynx, unlike other respiratory viruses that dwell in deeper regions of the lung.
Surprisingly, ACE2 expression in the lung is very low: it is limited to a few molecules per cell in the alveolar cells (AT2 cells) deep in the lung. But a just published paper by the Human Cell Atlas (HCA) consortium reports that ACE2 is highly expressed in some type of (secretory) cells of the inner nose!
Major route of viral entry is likely via large droplets that land in the nose — where expression of the viral entry receptor, ACE2 is highest. This is the transmission route that could be effectively blocked already by simple masks that provide a physical barrier.
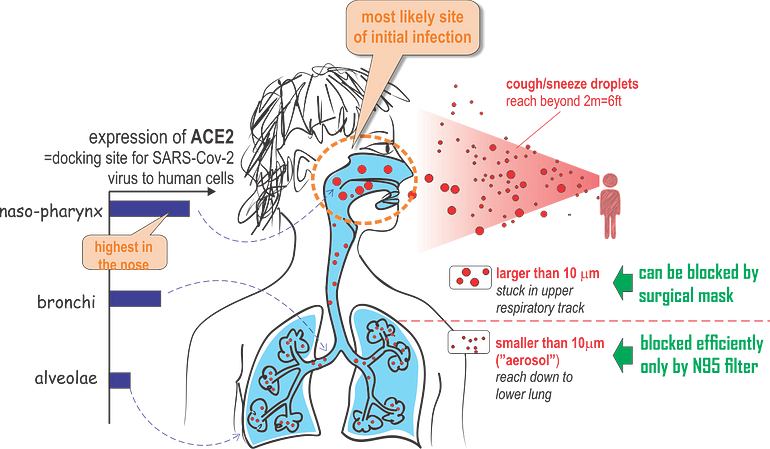
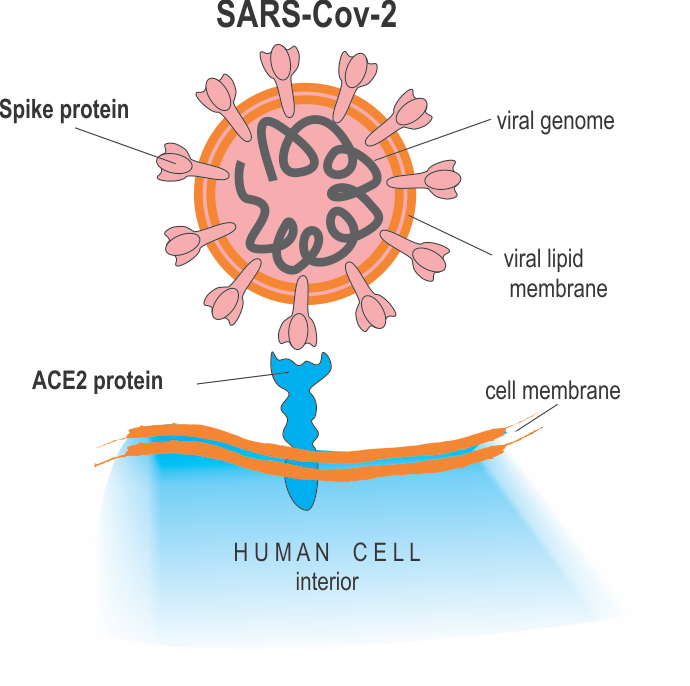
SARS-Cov-2 virus, like any virus, must dock onto human cells using a key-lock principle, in which the virus presents the key and the cell the lock that is complementary to the key to enter the cell and replicate. For the SARS-Cov-2 virus, the viral surface protein “Spike protein S” is the “key” and it must fit snugly into the “lock” protein that is expressed (=molecularly presented) on the surface of the host cells. The cellular lock protein that the SARS-Cov-2 virus uses is the ACE2 protein
SARS-Cov-2 enters the host cell by docking with its Spike protein to the ACE2 (blue) protein in cell surfaces:
Filtering effect for small droplets (aerosols) by various masks; home-made of tea cloth, surgical mask (3M “Tie-on”) and a FFP2 (N95) respirator mask. The numbers are scaled to the reference of 100 (source of droplets) for illustrative purposes, calculated from the PF (protection factor) values
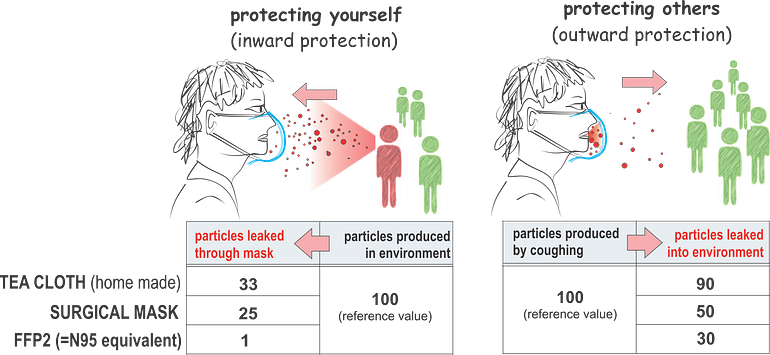
The tacit notion at the CDC that the alveolae are the destination site for droplets to deliver the virus load (the alveolae are after all the anatomical site of life-threatening pneumonia), has elevated the apparent importance of N95 masks and led to the dismissal of surgical masks.
Why N95 masks are much better over the surgical masks
In the case of the SARS-Cov-2 virus it is not known what the minimal infectious load is (number of viral particles needed to start the pathogenesis cascade that causes a clinical disease).
Minimal infectious load
Of course many aerosol droplets in the exhalation or cough spray may not contain the virus, but some will do.
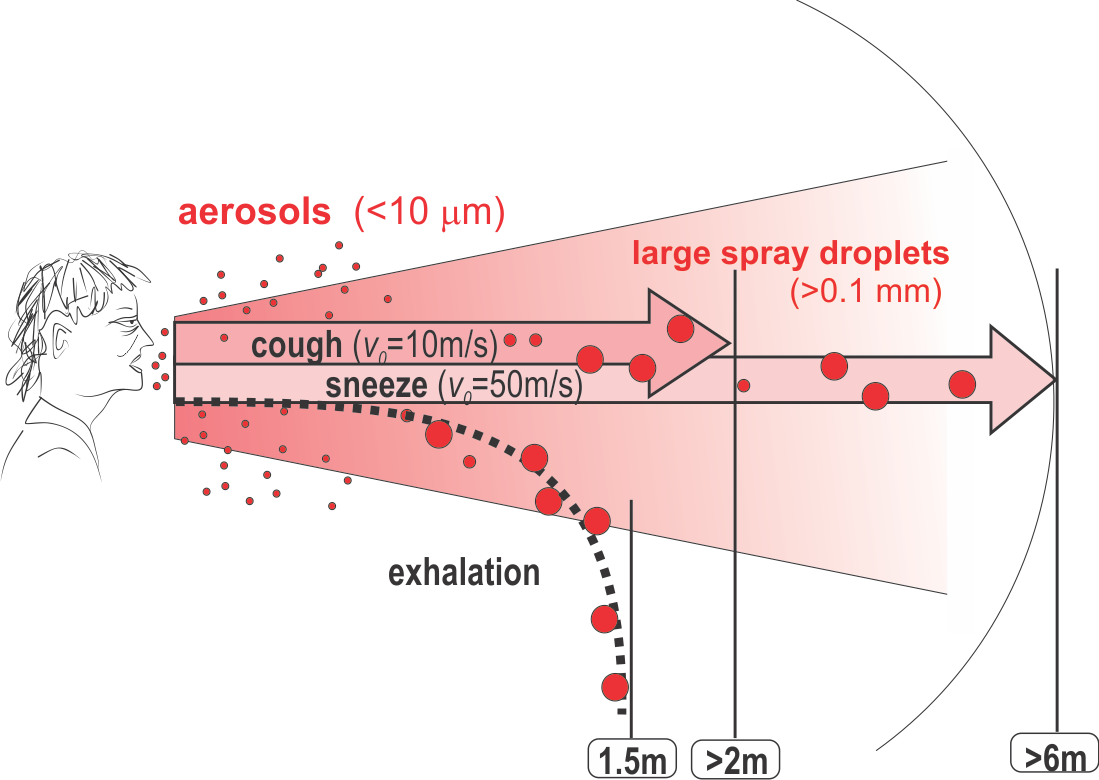
droplets of a typical cough expulsion have a size distribution such that approximately half of the droplet are in the categories of aerosols, albeit they collectively represent only less than 1/100,000 of the expelled volume
Droplets of a typical cough
For airborne particles to be inspired and reach deep into the lung, through all the air ducts down to the alveolar cells where gas-exchange takes place, it has to be small
Only droplets < 10 um can reach to alveolae (deep into lung). Larger droplets stuck in the nose, throat, upper air ducts of the lung, trachea and large bronchia.

Droplets can (for this discussion) be crudely divided in two large categories based on size
2 categories of droplets:
a) Droplets < 10 um: upper size limit of aerosol. Can float in the air/rooms by ventilation or winds and can be filtered (to 95%) by N95 favial masks (droplets < than 0.3 um). Here the surgical masks cannot help.
b) Droplets > 10 um (reaching 100+ um): called as spray droplets. Can be even visible by human from coughing/sneezing (0.1+ um).
Droplet larger than aerosols, when exhaled (at velocity of <1m/s), evaporate or fall to the ground less than 1.5 m away. When expelled at high velocity through coughing or sneezing, especially larger droplets (> 0.1 micrometers), can be carried by the jet more than 2m or 6m, respectively, away.
unidad_COVID2019
PMID: 31987001
DOI: 10.1080/22221751.2020.1719902
unidad_COVID2019
PMID: 31978945
DOI: 10.1056/NEJMoa2001017
unidad_COVID2019
PMID: 31991541
DOI: 10.3390/v12020135
Ancestor of all animals identified in Australian fossils
Summary:
unidad_COVID2019
unidad_COVID2019
unidad_COVID2019
unidad_COVID2019
unidad_COVID2019
unidad_COVID2019
Typically, double terminators are used to stop transcription. Because these parts can be up to ∼168 bp of DNA, this use of double terminators can lead to homologous recombination when used at multiple locations in a design
double terminators
Did you test the double terminator strength against your library?
there is littleelse on this list which can be considered part of a life history strategy if ‘life history’ is meant to be anchored in evolutionary biological research
Isn't altruism, the willingness and ability to sacrifice for kin, the rate of drop-off of willing altruism, etc all directly connected to evolutionary biology?
A spacer could compensate for any steric hindrance effect on recruiting the transcriptional machinery at the promoter of the next module in the assembly line; such an effect could be induced by the supercoiling that results when the transcription of the previous module is taking place. However, there is no direct evidence that this may cause a problem, and therefore the argument in favor of using a spacer remains speculative.